
The Human Microbiome
What is the Human Microbiome?
Hi readers, welcome to the first official post! What better topic to start off with than clarifying what the microbiome actually is, for those of you who aren’t familiar?! According to Jack Gilbert and his research team’s “Current understanding of the human microbiome,” the human microbiome may be defined as the community of microorganisms as well as their genetic information within the human body. This includes bacteria, archaea, viruses, fungi, and some protozoans. In fact, the number of bacterial cells in the human body actually outnumbers the human cell count! According to Kara Rogers in her article on the human microbiome, there are roughly 75-200 trillion individual bacteria in the human body with roughly 160 different bacterial species present within the gut alone.
I know what you may be thinking, this sounds like an invasion of the same scary organisms that cause infection. Although partially true, these microorganisms are also essential for our health and well-being. According to Rogers, a few of the many benefits of the human microbiota include aiding the breakdown of food and absorption nutrients in the gut, inhibiting the colonization of harmful bacteria, improving drug metabolism, and promoting skin health. Gilbert also notes that ongoing improvements in DNA sequencing technology for microbial communities has improved the scientific understanding of the human microbiome’s function and structure in diseased and healthy states. Recent studies have even linked the gut microbiome to obesity, cancer, inflammatory bowel disease, arthritis, depression, and many other diseases. Such research will continue to influence nutritional and lifestyle recommendations as well as diagnostic and therapeutics research. After all, like everything in life, the human microbiome is incredibly dynamic, shaped by factors such as diet, lifestyle, and the environment.
How does the Gut Microbiome Communicate Throughout the Body?
As we’ve mentioned, the gut microbiome plays a powerful role in human health. So, this must have some connection with the control center of our body, otherwise known as the brain. According to Marilia Carabotti’s article published in the Annals of Gastroenterology, this physical, bidirectional connection is known as the gut-brain axis (GBA), which allows communication between the central and enteric nervous system. In other words, through neural and hormonal signals, the GBA links the the brain with gastrointestinal functions and the gut microbiome. For those of you neuroscientists out there, the hypothalamic pituitary adrenal (HPA) axis plays a primary role in this connection. This bidirectional connection was further explained by Xiaomei Cong as allowing
top-down signaling from the brain to influence the motor, sensory and secretory modalities of the GI tract, and conversely, bottom-up signaling from the gut to affect brain function, especially [regions of the brain] devoted to emotion and stress.
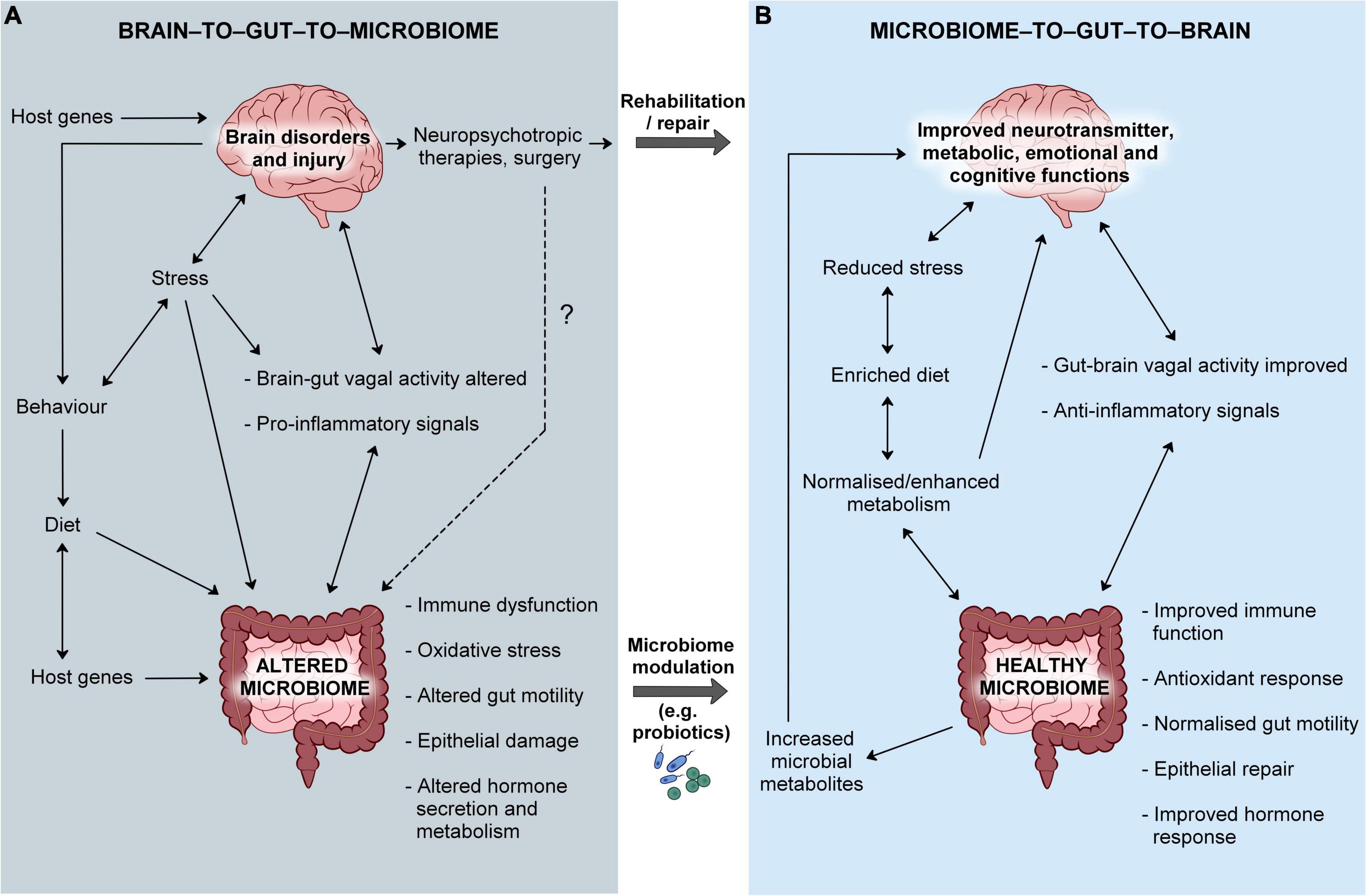
Carolina Costa and her team’s research contextualizes the significance of the GBA, noting that the gut microbiome impacts cognition, personality, and overall psychological health. It is also linked to anxiety, depression, autism, dementia, and a range of other neurological disorders. Stress hormones released through the HPA axis, in turn altar gut microbiome composition, likely by increasing intestinal permeability. Neurotransmitters also play a key role in this connection, impacting the gut and its microbiome by altering blood circulation, nutrient absorption, and the gastrointestinal immune system. Although this GBA is a complicated network, I encourage you to review the diagram above for a visual depiction of its components and bidirectional nature.
What Makes A Healthy Microbiome?
Although I have hinted at the intricacies of the human microbiome throughout this post, this question might be the most complex of them all. However, it is one of great importance and possibly the reason you landed on this blog in the first place! First off, it is important to note that there isn’t one set of microbes that comprise the “ideal microbiome” for every individual. According to an article by Jason Lloyd-Price, many large-scale studies have diverse ranges of microbial compositions in healthy populations, each influenced by geography, diet, and lifestyle. However, a healthy gut microbiome consists primarily of two bacteria phyla: Bacteroidetes and Firmicutes. The mouth of a healthy individual is dominated by several Streptococcus species and the skin with Corynebacterium, Propionibacterium, and Staphylococcus. Further taxonomic specifics can be noted in the figure below. Overall, diversity and stability within the microbiome are key!

Lloyd-Price further explains that the “core” healthy microbiome may also be defined in terms of key functions. This includes the microbiota’s ability to conduct necessary housekeeping functions for all microbes (transcription and translation, reproduction, energy production, etc) as well as the ability to thrive in the human body (host-cell adhesion, production of compounds to maintain host-microbe mutualism). Specialized functions are also crucial, as noted in the figure below. Lloyd-Price more specifically defines key gut microbiome functions including,
glycosaminoglycan biodegradation, the production of several short-chain fatty acids, enrichment for specific lipopolysaccharides, and the production of vitamins and essential amino acids.

A healthy microbiome is established prior to birth through the placenta and exposure to the birth canal. Breast milk and early nutrition are also key in promoting a healthy microbiome among infants. A diet rich in fiber and probiotics is crucial in achieving the optimal microbiome. According to Megan Dix’s article on gut health, fiber-rich foods include legumes, whole grains, and lots of fruits and vegetables. Fermented foods are a healthy source of probiotics. Also in terms of diet, it is important to limit added sugar and processed foods as these harm the gut microbiome and lead to inflammation. Stress-management, improving sleep quality, and ensuring adequate hydration are other key strategies to maximize the health of your microbiome.
